Quick Overview
Associated References
Main Article
History
The use of iodine in wound care has a rich historical context, evolving significantly since its discovery in the early 19th century. Elemental iodine was first isolated in 1811 by Bernard Courtois, and its antiseptic properties were recognized shortly thereafter, leading to widespread adoption in medical practice. Povidone-iodine (PVP-I), a complex of iodine and a polymer, was developed in the 1950s, providing a stable and less irritating alternative to elemental iodine for topical antisepsis. This formulation has become a cornerstone in wound management due to its broad-spectrum antimicrobial activity and minimal cytotoxicity to surrounding tissues (Bigliardi et al., 2017). The historical trajectory of iodine in wound care reflects a growing understanding of its efficacy and safety, paving the way for its current applications in various clinical settings.
Mechanism of Action of Iodine in Wound Care
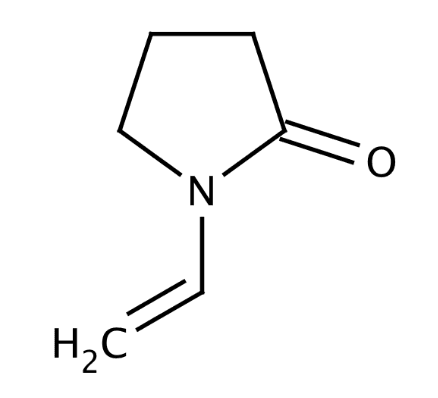
The mechanism of action of iodine, particularly in the form of povidone-iodine (PVP-I), is multifaceted and involves both chemical and biological processes that contribute to its effectiveness as an antimicrobial agent in wound care. PVP-I is a complex of iodine and polyvinylpyrrolidone (PVP), which serves as a carrier that enhances the solubility and stability of iodine in aqueous solutions. This formulation allows for the controlled release of free iodine, which is the active antimicrobial component Niu et al. (2021)Lee et al., 2005).
Antimicrobial Activity
The primary mechanism by which iodine exerts its antimicrobial effects is through the oxidation of cellular components within microorganisms. Iodine penetrates the cell walls of bacteria, fungi, and viruses, leading to the disruption of essential cellular functions. This includes the oxidation of proteins and nucleic acids, which ultimately results in cell death (Durani & Leaper, 2008; Bigliardi et al., 2017). The broad-spectrum activity of iodine is particularly significant; it has been shown to be effective against a wide variety of pathogens, including antibiotic-resistant strains such as methicillin-resistant Staphylococcus aureus (MRSA) (Allam et al., 2019; Hoekstra et al., 2016).
Moreover, iodine’s efficacy extends to biofilm-forming bacteria, which are often implicated in chronic wound infections. Studies have demonstrated that PVP-I can effectively reduce biofilm formation by disrupting the extracellular matrix that protects bacterial colonies, thereby enhancing the susceptibility of these pathogens to antimicrobial agents (Junka et al., 2013; Hoekstra et al., 2016). This is particularly important in chronic wounds, where biofilms can impede healing and contribute to persistent infections (Durani & Leaper, 2008; Hoekstra et al., 2016).
Promotion of Wound Healing
In addition to its antimicrobial properties, iodine plays a role in promoting wound healing. Research indicates that PVP-I can enhance the healing process by stimulating the inflammatory response and promoting re-epithelialization and granulation tissue formation (Gwak et al., 2019; Bigliardi et al., 2017). The presence of iodine has been associated with increased levels of transforming growth factors (TGF), which are crucial for cell proliferation and tissue repair (Gwak et al., 2019). Furthermore, the moist environment created by iodine-based dressings is conducive to healing, as it prevents desiccation and supports cellular migration across the wound bed (Bigliardi et al., 2017; Langer et al., 2006).
The liposomal formulation of PVP-I has been shown to improve the distribution and penetration of iodine into the skin and hair follicles, further enhancing its therapeutic effects (Langer et al., 2006; Augustin et al., 2017). This formulation not only provides sustained antimicrobial activity but also helps maintain moisture levels in the wound, which is critical for optimal healing conditions (Langer et al., 2006; Augustin et al., 2017).
Cytotoxicity and Safety Profile
Despite its benefits, the use of iodine in wound care is not without concerns. High concentrations of iodine can exhibit cytotoxic effects on fibroblasts and keratinocytes, which are essential for wound healing (Luo, 2023; Durani & Leaper, 2008). However, studies have indicated that appropriately formulated PVP-I solutions, particularly those with lower concentrations of free iodine, can minimize these adverse effects while retaining antimicrobial efficacy (Lee et al., 2005; Bigliardi et al., 2017).
Clinical evidence supports the notion that PVP-I does not significantly impede the healing process when used correctly. For instance, cadexomer iodine, another iodine-based formulation, has been shown to promote healing in diabetic foot ulcers, suggesting that iodine can be beneficial when used in a controlled manner (Gwak et al., 2019; Bigliardi et al., 2017).
In summary, the mechanism of action of iodine in wound care encompasses its potent antimicrobial properties, its ability to disrupt biofilms, and its role in enhancing the wound healing process. While safety concerns regarding cytotoxicity exist, careful formulation and application can mitigate these risks, making iodine a valuable agent in the management of wounds.
References:
- Allam, A., Abotakia, T., & Farghally, M. (2019). Povidone-iodine 3.35% solution versus normal saline for irrigation in lumbar fusion surgery: a retrospective study. Egyptian Spine Journal, 30(1), 48-56. https://doi.org/10.21608/esj.2019.5477.1069
- Alves, P., Barreto, R., Barrois, B., Gryson, L., Meaume, S., & Monstrey, S. (2020). Update on the role of antiseptics in the management of chronic wounds with critical colonisation and/or biofilm. International Wound Journal, 18(3), 342-358. https://doi.org/10.1111/iwj.13537
- Augustin, M., Goepel, L., Jacobi, A., Bosse, B., Müeller, S., & Hopp, M. (2017). Efficacy and tolerability of liposomal polyvinylpyrrolidone-iodine hydrogel for the localized treatment of chronic infective, inflammatory, dermatoses: an uncontrolled pilot study. Clinical Cosmetic and Investigational Dermatology, Volume 10, 373-384. https://doi.org/10.2147/ccid.s141887
- Bigliardi, P., Alsagoff, S., Elkafrawi, H., Pyon, J., Wa, C., & Villa, M. (2017). Povidone iodine in wound healing: a review of current concepts and practices. International Journal of Surgery, 44, 260-268. https://doi.org/10.1016/j.ijsu.2017.06.073
- Bigliardi, P., Alsagoff, S., Elkafrawi, H., Pyon, J., Wa, C., & Villa, M. (2017). Povidone iodine in wound healing: a review of current concepts and practices. International Journal of Surgery, 44, 260-268. https://doi.org/10.1016/j.ijsu.2017.06.073
- Bigliardi, P., Langer, S., Cruz, J., Kim, S., Nair, H., & Srisawasdi, G. (2017). An asian perspective on povidone iodine in wound healing. Dermatology, 233(2-3), 223-233. https://doi.org/10.1159/000479150
- Durani, P. and Leaper, D. (2008). Povidone–iodine: use in hand disinfection, skin preparation and antiseptic irrigation. International Wound Journal, 5(3), 376-387. https://doi.org/10.1111/j.1742-481x.2007.00405.x
- Gwak, H., Han, S., Lee, J., Park, S., Sung, K., Kim, S., … & Chung, H. (2019). Efficacy of a povidone‐iodine foam dressing (betafoam) on diabetic foot ulcer. International Wound Journal, 17(1), 91-99. https://doi.org/10.1111/iwj.13236
- Hoekstra, M., Westgate, S., & Müeller, S. (2016). Povidone‐iodine ointment demonstrates in vitro efficacy against biofilm formation. International Wound Journal, 14(1), 172-179. https://doi.org/10.1111/iwj.12578
- Junka, A., Bartoszewicz, M., Smutnicka, D., Secewicz, A., & Szymczyk, P. (2013). Efficacy of antiseptics containing povidone‐iodine, octenidine dihydrochloride and ethacridine lactate against biofilm formed by pseudomonas aeruginosa and staphylococcus aureus measured with the novel biofilm‐oriented antiseptics test. International Wound Journal, 11(6), 730-734. https://doi.org/10.1111/iwj.12057
- Kang, D., Ma, C., & Park, N. (2022). Antiseptic povidone–iodine heals the grain boundary of perovskite solar cells. Acs Applied Materials & Interfaces, 14(7), 8984-8991. https://doi.org/10.1021/acsami.1c21479
- Langer, S., Botteck, N., Bosse, B., Reimer, K., Vogt, P., Steinau, H., … & Müeller, S. (2006). Effect of polyvinylpyrrolidone-iodine liposomal hydrogel on wound microcirculation in skh1-<i>hr</i> hairless mice. European Surgical Research, 38(1), 27-34. https://doi.org/10.1159/000091524
- Lee, S., Zhai, H., & Maibach, H. (2005). Allergic contact dermatitis from iodine preparations: a conundrum. Contact Dermatitis, 52(4), 184-187. https://doi.org/10.1111/j.0105-1873.2005.00499.x
- Luo, Y. (2023). Effectiveness of continuous home wound care on patients with diabetic foot ulcers. Journal of Advanced Nursing, 80(8), 3395-3413. https://doi.org/10.1111/jan.16039
- Mthanti, S., Pelle, G., & Cremers, N. (2022). L-mesitran foam: evaluation of a new wound care product. Case Reports in Dermatological Medicine, 2022, 1-5. https://doi.org/10.1155/2022/4833409
- Niu, X., Wan, S., Rong, X., Mei, L., Mehwish, N., & Lee, B. (2021). Facile fabrication of povidone iodine‐embedded polytetrafluoroethylene superhydrophobic films with improved antiadhesive and bactericidal properties in bacterial environments. Macromolecular Materials and Engineering, 306(9). https://doi.org/10.1002/mame.202100193
- Roshan, M. (2024). Hypochlorous acid -the future of wound care?. Journal of the Pakistan Medical Association, 74(4), 616-616. https://doi.org/10.47391/jpma.10290
- Stadio, A., Gambacorta, V., Cristi, M., Ralli, M., Pindozzi, S., Tassi, L., … & Ricci, G. (2019). The use of povidone‐iodine and sugar solution in surgical wound dehiscence in the head and neck following radio‐ International Wound Journal, 16(4), 909-915. https://doi.org/10.1111/iwj.13118
- Tiarasanti, F. (2024). The effects of potato (solanum tuberosum l. vs. granola; solanaceae) peel extract gel on gingival wound healing in wistar rats. Journal of Experimental Pharmacology, Volume 16, 25-35. https://doi.org/10.2147/jep.s443355
- Vogt, P., Hauser, J., Müeller, S., Bosse, B., & Hopp, M. (2017). Efficacy of conventional and liposomal povidone–iodine in infected mesh skin grafts: an exploratory study. Infectious Diseases and Therapy, 6(4), 545-555. https://doi.org/10.1007/s40121-017-0172-z
- Wang, L., Qin, W., Ya-ying, Z., Chen, B., Zhao, X., Zhao, H., … & Ning, J. (2017). Transforming growth factor β plays an important role in enhancing wound healing by topical application of povidone-iodine. Scientific Reports, 7(1). https://doi.org/10.1038/s41598-017-01116-5
- Yu, J., Wang, P., Yin, M., Zhang, K., Wang, X., & Han, B. (2022). Carboxymethyl chitosan-grafted polyvinylpyrrolidone-iodine microspheres for promoting the healing of chronic wounds. Bioengineered, 13(4), 8735-8746. https://doi.org/10.1080/21655979.2022.2054911