Quick Overview
Associated References
Associated Care Plans/Tutorials
Associated Products
Main Article
History of Hyaluronic Acid
Hyaluronic acid (HA) was first identified in 1934 by Karl Meyer and his colleagues at Columbia University, who isolated it from the vitreous body of bovine eyes. This discovery marked the beginning of understanding HA as a significant component of connective tissues in animals and humans alike (ramakrishnan et al., 2020). Over the decades, HA’s role expanded beyond its initial identification, with research demonstrating its presence in various tissues, including skin, cartilage, and synovial fluid, highlighting its importance in biological processes (Lin et al., 2013). The introduction of HA into medical and skincare practices began in the late 20th century, with its use as a dermal filler gaining traction in cosmetic dermatology due to its biocompatibility and ability to retain moisture (Jang et al., 2014). By the 1990s, HA was being utilized in various formulations for wound healing, leveraging its natural properties to enhance tissue repair and hydration (Makvandi et al., 2020).
Mechanism of Action
The mechanism of action of hyaluronic acid in wound healing is multifaceted. HA plays a crucial role in maintaining hydration within the extracellular matrix, which is essential for cellular proliferation and migration during the healing process (Kazkayası & Denizalti, 2023). Its high molecular weight allows it to attract and retain water, creating a moist environment conducive to healing (Francesco et al., 2022). Furthermore, HA promotes angiogenesis, the formation of new blood vessels, which is vital for delivering nutrients and oxygen to healing tissues (Francesco et al., 2022). Studies have shown that HA modulates inflammatory responses, reducing the infiltration of inflammatory cells and promoting re-epithelialization and granulation tissue formation (Francesco et al., 2022). The interaction of HA with cell surface receptors, such as CD44, facilitates cellular signaling pathways that enhance fibroblast activity and collagen synthesis, further contributing to tissue regeneration (Asparuhova et al., 2018).
Clinical Uses
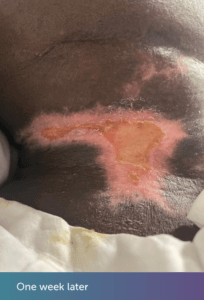
Hyaluronic acid has a wide range of clinical applications in both wound care and dermatology. In wound care, HA is particularly effective for managing chronic wounds, burns, and surgical incisions. Its ability to maintain moisture and promote granulation tissue formation makes it a valuable component in dressings and topical formulations (Kazkayası & Denizalti, 2023; Francesco et al., 2022). Clinical studies have demonstrated that HA-containing formulations significantly improve healing outcomes compared to conventional treatments or placebo (Kazkayası & Denizalti, 2023). In dermatology, HA is widely used in moisturizers, anti-aging treatments, and injectable fillers. Its hydrating properties help to restore skin elasticity and reduce the appearance of fine lines and wrinkles (Jang et al., 2014; Qiao et al., 2019). Injectable HA fillers, such as Juvederm and Restylane, have become popular for facial contouring and volumization, providing immediate aesthetic results with minimal downtime (Qiao et al., 2019; Kim, 2023).
Brands of Hyaluronic Acid Products
Several brands have emerged as leaders in the hyaluronic acid market, particularly in the fields of wound care and dermatology. Hyalofill is known for its advanced formulations designed for wound management, while Dermapure offers a range of HA-based skincare products aimed at hydration and anti-aging (Qiao et al., 2019). Juvederm, a well-known brand in the cosmetic industry, provides a variety of HA fillers tailored for different facial areas, ensuring versatility in aesthetic treatments (Qiao et al., 2019). These products leverage the unique properties of HA, such as its viscoelasticity and biocompatibility, to deliver effective results in both therapeutic and cosmetic applications (Kim, 2023).
Precautions for Use
While hyaluronic acid is generally considered safe, certain precautions must be taken to ensure its effective and safe use. Contraindications include known allergies to HA or any of its components, as well as active infections at the injection site (Jang et al., 2014). Potential allergic reactions, although rare, can occur and should be monitored closely (Jang et al., 2014). Proper application techniques are crucial, particularly in injectable forms, to minimize the risk of complications such as bruising or swelling (Jang et al., 2014). Healthcare professionals should also educate patients about the importance of post-treatment care to optimize outcomes and reduce the risk of adverse effects (Jang et al., 2014; Kim, 2023).
Conclusion
Hyaluronic acid represents a significant advancement in both wound care and dermatological applications. Its historical development, coupled with a deep understanding of its mechanisms of action, clinical uses, and available products, underscores its importance in modern medicine. As research continues to evolve, the potential applications of HA are likely to expand, further enhancing its role in promoting healing and improving aesthetic outcomes.
References:
- Asparuhova, M., Kiryak, D., Eliezer, M., Mihov, D., & Sculean, A. (2018). Activity of two hyaluronan preparations on primary human oral fibroblasts. Journal of Periodontal Research, 54(1), 33-45. https://doi.org/10.1111/jre.12602
- Francesco, F., Riccio, M., & Jimi, S. (2022). Contribution of topical agents such as hyaluronic acid and silver sulfadiazine to wound healing and management of bacterial biofilm. Medicina, 58(6), 835. https://doi.org/10.3390/medicina58060835
- Jang, J., Hong, K., & Choi, E. (2014). A case of nonthrombotic pulmonary embolism after facial injection of hyaluronic acid in an illegal cosmetic procedure. Tuberculosis and Respiratory Diseases, 77(2), 90. https://doi.org/10.4046/trd.2014.77.2.90
- Kazkayası, İ. and Denizalti, M. (2023). The effects of metformin and hyaluronic acid on wound healing in high glucose incubated fibroblast cells. Journal of Research in Pharmacy, 27(4)(27(4)), 1338-1345. https://doi.org/10.29228/jrp.421
- Kim, K. (2023). “cohesiveness of hyaluronic acid fillers”: evaluation using multiple cohesion tests. Archives of Plastic Surgery, 51(01), 014-019. https://doi.org/10.1055/a-2234-1019
- Lin, Q., Huang, X., Tang, J., & Chen, H. (2013). Facile and efficient anti-fouling surface construction on poly(dimethylsiloxane) via mussel-inspired chemistry. Advanced Materials Research, 749, 344-349. https://doi.org/10.4028/www.scientific.net/amr.749.344
- Makvandi, P., Caccavale, C., Sala, F., Zeppetelli, S., Veneziano, R., & Borzacchiello, A. (2020). Natural formulations provide antioxidant complement to hyaluronic acid-based topical applications used in wound healing. Polymers, 12(8), 1847. https://doi.org/10.3390/polym12081847
- Qiao, J., Jia, Q., Jin, H., Li, F., He, C., Yang, J., … & Fu, L. (2019). Long-term follow-up of longevity and diffusion pattern of hyaluronic acid in nasolabial fold correction through high-frequency ultrasound. Plastic & Reconstructive Surgery, 144(2), 189e-196e. https://doi.org/10.1097/prs.0000000000005848
- ramakrishnan, D., gouthaman, S., & Periasamy, S. (2020). Effect of hyaluronic acid cream in management of maxillofacial wounds. International Journal of Research in Pharmaceutical Sciences, 11(4), 6892-6896. https://doi.org/10.26452/ijrps.v11i4.3672