Quick Overview
Associated References
Associated Care Plans/Tutorials
Associated Products
Main Article
History
Foam dressings have undergone significant evolution since their inception, initially emerging as a response to the need for more effective wound management solutions. The development of polyurethane foam dressings in the late 20th century marked a pivotal moment in wound care, as these materials were designed to address the limitations of traditional dressings, such as gauze and film. Early studies highlighted the advantages of foam dressings in managing exudate and maintaining a moist wound environment, crucial for optimal healing (Kowalczuk et al., 2020; Hargis, 2024). Over the years, advancements in material science have led to the incorporation of antimicrobial agents and enhanced moisture management properties, further expanding the clinical applications of foam dressings (Tiscar-González et al., 2021; Pak et al., 2018).
The introduction of silver-releasing foam dressings in the early 2000s represented a significant milestone, as these products combined the benefits of moisture retention with antimicrobial properties, addressing the growing concern of wound infections (Wang et al., 2021; Salisbury et al., 2022). Recent innovations have included the development of multilayered foam dressings that offer improved absorption and cushioning, catering to a wide range of wound types, from acute surgical wounds to chronic ulcers (Hargis, 2024; Tiscar-González et al., 2021). The continuous research and clinical trials conducted over the past decade have solidified the role of foam dressings as a standard in modern wound care practices (Zhang et al., 2023; Park et al., 2023).
Mechanism of Action
Foam dressings operate through several mechanisms that facilitate wound healing. Primarily, they are designed to absorb exudate, which is critical in preventing maceration of surrounding tissues and promoting a moist wound environment (Kowalczuk et al., 2020; Yamane et al., 2013). The porous structure of polyurethane foam allows for high fluid retention while maintaining a balance of moisture, which is essential for cellular migration and tissue regeneration (Hasatsri et al., 2018; Zhang, 2024). This moisture-retentive capability not only aids in autolytic debridement but also helps to regulate the temperature at the wound site, creating an optimal healing environment (Hargis, 2024; Tiscar-González et al., 2021).
Additionally, foam dressings provide cushioning and protection to the wound, reducing pain and discomfort associated with pressure and friction (Hargis, 2024; Woo & Heil, 2017). The mechanical properties of foam allow it to conform to the wound bed, distributing pressure evenly and minimizing shear forces, which are particularly beneficial for patients at risk of pressure ulcers (Yoshimura et al., 2016; Kohta et al., 2022). Furthermore, certain foam dressings are impregnated with antimicrobial agents, such as silver or iodine, which help to reduce bacterial load and prevent infection, thereby enhancing the overall healing process (Wang et al., 2021; Salisbury et al., 2022; Lázaro‐Martínez et al., 2019).
Clinical Uses
Foam dressings are versatile and suitable for a variety of wound types, including pressure ulcers, surgical wounds, and exuding wounds. Their ability to manage moderate to heavy exudate makes them particularly effective for chronic wounds, such as diabetic foot ulcers and venous leg ulcers, where exudate management is crucial for healing (Pak et al., 2018; Zhang et al., 2023; Gwak et al., 2019). Clinical studies have demonstrated that foam dressings can significantly improve healing rates and reduce complications in patients with pressure injuries compared to traditional dressings (Zhang et al., 2023; Park et al., 2023).
In surgical settings, foam dressings are often employed post-operatively to protect incisions while allowing for drainage, thus minimizing the risk of infection and promoting faster recovery (Tiscar-González et al., 2021; Woo & Heil, 2017). The cushioning effect of foam dressings also makes them ideal for use in areas prone to friction and shear, such as the sacral region in bedridden patients (Yoshimura et al., 2016; Kohta et al., 2022). Moreover, their adaptability to various anatomical sites, including complex and irregular wounds, further underscores their clinical utility (Zhang, 2024; Yang & Hu, 2018).
Brands of Foam Dressings
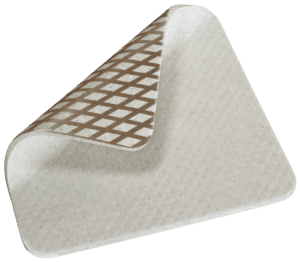
Several brands of foam dressings are widely recognized in clinical practice, each offering unique features tailored to specific wound care needs. Mepilex, for instance, is known for its soft silicone technology that minimizes pain during dressing changes while providing effective exudate management (Hargis, 2024; Tiscar-González et al., 2021). Allevyn, another popular brand, combines a hydrocellular foam structure with a waterproof backing, making it suitable for a range of wound types, including those requiring moisture control and infection prevention (Pak et al., 2018; Zhang et al., 2023).
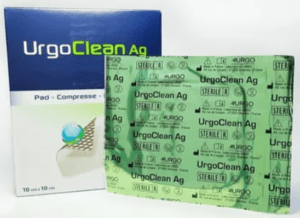
Biatain foam dressings are particularly notable for their silver-releasing properties, which enhance antimicrobial efficacy while maintaining a moist environment (Wang et al., 2021; Lázaro‐Martínez et al., 2019). Additionally, Betafoam, a povidone-iodine impregnated dressing, has gained attention for its dual action of exudate absorption and infection control, making it a valuable option for diabetic foot ulcers (Gwak et al., 2019; Park et al., 2023). These brands exemplify the advancements in foam dressing technology, reflecting a commitment to improving patient outcomes in wound care.
Precautions for Safe and Effective Use
While foam dressings offer numerous benefits, healthcare professionals must consider specific precautions to ensure their safe and effective use. One critical consideration is the assessment of wound type; foam dressings are generally contraindicated for dry wounds, where moisture retention may exacerbate the condition (Tiscar-González et al., 2021; Hasatsri et al., 2018). Additionally, the frequency of dressing changes should be tailored to the level of exudate, as excessive moisture can lead to maceration and delayed healing (Tiscar-González et al., 2021; Lee et al., 2017).
Potential complications associated with foam dressings include allergic reactions to materials, particularly in patients with sensitivities to polyurethane or silicone (Hargis, 2024; Woo & Heil, 2017). Regular monitoring of the wound site is essential to detect signs of infection or adverse reactions promptly. Furthermore, clinicians should educate patients on the importance of adhering to dressing change protocols and recognizing changes in their wounds that may necessitate medical attention (Lee et al., 2017; Yoshimura et al., 2016).
In conclusion, foam dressings represent a significant advancement in wound care, offering a range of benefits that enhance healing outcomes. Their ability to absorb exudate, provide cushioning, and maintain a moist environment makes them suitable for various wound types. As the field of wound management continues to evolve, ongoing research and innovation will undoubtedly lead to further improvements in foam dressing technology and application.
References:
- Gwak, H., Han, S., Lee, J., Park, S., Sung, K., Kim, S., … & Chung, H. (2019). Efficacy of a povidone‐iodine foam dressing (betafoam) on diabetic foot ulcer. International Wound Journal, 17(1), 91-99. https://doi.org/10.1111/iwj.13236
- Hargis, A. (2024). Foam dressings for wound healing. Current Dermatology Reports, 13(1), 28-35. https://doi.org/10.1007/s13671-024-00422-2
- Hasatsri, S., Pitiratanaworanat, A., Swangwit, S., Boochakul, C., & Tragoonsupachai, C. (2018). Comparison of the morphological and physical properties of different absorbent wound dressings. Dermatology Research and Practice, 2018, 1-6. https://doi.org/10.1155/2018/9367034
- Kohta, M., Urai, T., Saad, S., & Sugama, J. (2022). Multilayered silicone foam dressings potentially used for preventing recurrence of pressure injuries: a bench‐to‐clinical bedside study. Japan Journal of Nursing Science, 20(1). https://doi.org/10.1111/jjns.12504
- Kowalczuk, D., Miazga-Karska, M., Gładysz, A., Warda, P., Barańska, A., & Drop, B. (2020). Characterization of ciprofloxacin-bismuth-loaded antibacterial wound dressing. Molecules, 25(21), 5096. https://doi.org/10.3390/molecules25215096
- Lee, S., Sim, S., Ki, S., Choi, J., & Kim, H. (2017). Novel dressing method of fixing polyurethane foam on the soft tissue defect of the finger. Journal of Wound Management and Research, 13(2), 44-48. https://doi.org/10.22467/jwmr.2017.00185
- Lázaro‐Martínez, J., Álvaro‐Afonso, F., Fernández, D., Molines-Barroso, R., García‐Álvarez, Y., & García-Morales, E. (2019). Clinical and antimicrobial efficacy of a silver foam dressing with silicone adhesive in diabetic foot ulcers with mild infection. The International Journal of Lower Extremity Wounds, 18(3), 269-278. https://doi.org/10.1177/1534734619866610
- Pak, C., Park, D., Oh, T., Lee, W., Jun, Y., Lee, K., … & Rhie, J. (2018). Comparison of the efficacy and safety of povidone‐iodine foam dressing (betafoam), hydrocellular foam dressing (allevyn), and petrolatum gauze for split‐thickness skin graft donor site dressing. International Wound Journal, 16(2), 379-386. https://doi.org/10.1111/iwj.13043
- Park, K., Baek, K., Kim, M., Ju, M., Jung, W., & Yoon, Y. (2023). A prospective, randomized, non-inferiority trial to compare the efficacy of 3% povidone-iodine foam dressing and silver foam dressing in the treatment of pressure injuries. Journal of Wound Management and Research, 19(1), 13-20. https://doi.org/10.22467/jwmr.2023.02376
- Salisbury, A., Mullin, M., Foulkes, L., Chen, R., & Percival, S. (2022). Controlled‐release iodine foam dressings demonstrate broad‐spectrum biofilm management in several in vitro models. International Wound Journal, 19(7), 1717-1728. https://doi.org/10.1111/iwj.13773
- Tiscar-González, V., Menor-Rodríguez, M., Rabadán-Sainz, C., Fraile-Bravo, M., Styche, T., Valenzuela-Ocaña, F., … & Muñoz-García, L. (2021). Clinical and economic impact of wound care using a polyurethane foam multilayer dressing. Advances in Skin & Wound Care, 34(1), 23-30. https://doi.org/10.1097/01.asw.0000722744.20511.71
- Wang, Y., Lee, H., Chen, C., Kuo, M., Ramachandran, S., Chen, R., … & Kuo, Y. (2021). The effects of silver-releasing foam dressings on diabetic foot ulcer healing. Journal of Clinical Medicine, 10(7), 1495. https://doi.org/10.3390/jcm10071495
- Woo, K. and Heil, J. (2017). A prospective evaluation of methylene blue and gentian violet dressing for management of chronic wounds with local infection. International Wound Journal, 14(6), 1029-1035. https://doi.org/10.1111/iwj.12753
- Yamane, T., Nakagami, G., Yoshino, S., Muramatsu, A., Matsui, S., Oishi, Y., … & Sanada, H. (2013). Hydrocellular foam dressing promotes wound healing along with increases in hyaluronan synthase 3 and pparα gene expression in epidermis. Plos One, 8(8), e73988. https://doi.org/10.1371/journal.pone.0073988
- Yang, Y. and Hu, H. (2018). Application of superabsorbent spacer fabrics as exuding wound dressing. Polymers, 10(2), 210. https://doi.org/10.3390/polym10020210
- Yoshimura, M., Ohura, N., Tanaka, J., Ichimura, S., Kasuya, Y., Hotta, O., … & Suzuki, N. (2016). Soft silicone foam dressing is more effective than polyurethane film dressing for preventing intraoperatively acquired pressure ulcers in spinal surgery patients: the border operating room spinal surgery (boss) trial in japan. International Wound Journal, 15(2), 188-197. https://doi.org/10.1111/iwj.12696
- Zhang, C., Zhang, S., Wu, B., Zhang, K., & Chen, H. (2023). Efficacy of different types of dressings on pressure injuries: systematic review and network meta‐ Nursing Open, 10(9), 5857-5867. https://doi.org/10.1002/nop2.1867
- Zhang, G. (2024). Effects of different dressings in the prevention of facial skin pressure injury related to non‐invasive ventilation: systematic review and network meta‐ International Wound Journal, 21(2). https://doi.org/10.1111/iwj.14678