Quick Overview
Associated References
Main Article
Corticosteroids have a long and complex history in medicine, particularly in the context of wound care. Initially discovered in the 1940s, corticosteroids were recognized for their potent anti-inflammatory properties, leading to their widespread use in various medical conditions, including skin disorders and wound management. The active ingredient, cortisone, was first isolated from the adrenal cortex and subsequently synthesized, paving the way for the development of synthetic corticosteroids. Over the decades, the understanding of corticosteroids’ mechanisms of action and their effects on wound healing has evolved significantly. While they are effective in reducing inflammation and managing pain, their role in wound care has been scrutinized due to their potential to impair healing processes, particularly in chronic wounds and surgical sites (Arai et al., 2020; Kaufman et al., 2014).
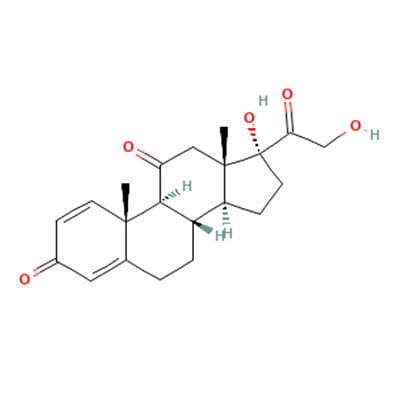
The mechanism of action of corticosteroids primarily involves the modulation of inflammatory responses. Corticosteroids exert their effects by binding to glucocorticoid receptors, leading to the transcription of anti-inflammatory proteins and the suppression of pro-inflammatory cytokines. This action results in a decrease in neutrophil infiltration, reduced fibroblast proliferation, and impaired collagen synthesis, all of which are critical for effective wound healing (Kaufman et al., 2014; Wu et al., 2019). Specifically, corticosteroids inhibit the inflammatory phase of wound healing, which is essential for the transition to the proliferative phase. This inhibition can lead to delayed epithelialization, reduced angiogenesis, and inadequate collagen deposition, ultimately resulting in impaired wound healing (Faith et al., 2021; Coppola et al., 2018; Zinder et al., 2019).
Precautions must be taken when using corticosteroids in wound care. The systemic and local effects of corticosteroids can lead to complications, particularly in patients with pre-existing conditions such as diabetes or those undergoing surgical procedures. For instance, studies have shown that corticosteroid use is associated with an increased risk of anastomotic leakage following gastrointestinal surgeries, highlighting the need for careful patient selection and monitoring (Eriksen et al., 2014). Additionally, the timing of corticosteroid administration is crucial; early administration post-injury can exacerbate healing delays, while their use in chronic wounds may necessitate a reevaluation of treatment strategies to optimize healing outcomes (Wang et al., 2018).
The adverse effects of corticosteroids on wound healing are well-documented. Research indicates that corticosteroids can lead to incomplete granulation tissue formation and reduced wound contraction, which are vital for the closure of wounds (Kaufman et al., 2014; Ojeh et al., 2020). Furthermore, the use of topical corticosteroids has been shown to delay the healing of corneal injuries and other epithelial wounds, underscoring the need for caution in their application (Wu et al., 2019; Hagedorn et al., 2020). In contrast, alternative treatments, such as the use of retinoids, have been suggested to mitigate some of the negative effects associated with corticosteroids by promoting collagen synthesis and enhancing re-epithelialization (Jain et al., 2015; Politis et al., 2016).
In the context of specific wound types, such as hypertrophic scars and keloids, corticosteroids have been employed therapeutically, albeit with mixed results. While intralesional corticosteroid injections can reduce scar formation, their efficacy varies, and recurrence rates remain a concern (Coppola et al., 2018; Suter et al., 2017). The use of corticosteroids in treating infantile hemangiomas has also been explored, with studies indicating that while they can be effective, they do not consistently outperform other treatment modalities (Faith et al., 2021; Wang et al., 2018).
The historical context of corticosteroids in wound care reflects a broader understanding of their pharmacological properties and clinical implications. As research continues to evolve, it is essential for clinicians to remain informed about the benefits and risks associated with corticosteroid use in wound management. This knowledge will enable them to make informed decisions regarding patient care and treatment planning, ultimately improving patient outcomes in wound healing (Croft et al., 2015; Muñoz & Posthauer, 2021).
In summary, corticosteroids play a significant role in wound care, primarily due to their anti-inflammatory properties. However, their use must be approached with caution, considering the potential for impaired healing and other complications. Understanding the mechanisms of action, historical context, and precautions associated with corticosteroids will empower clinicians to navigate the complexities of wound management effectively. Continued education and research are vital to optimizing the use of corticosteroids in clinical practice, ensuring that patient care remains at the forefront of nursing practice.
References:
- Arai, K., Yamamoto, K., Suzuki, T., Mitsukawa, N., & Ishii, I. (2020). Risk factors affecting pressure ulcer healing: impact of prescription medications. Wound Repair and Regeneration, 28(3), 409-415. https://doi.org/10.1111/wrr.12791
- Coppola, M., Salzillo, R., Segreto, F., & Persichetti, P. (2018). Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clinical Cosmetic and Investigational Dermatology, Volume 11, 387-396. https://doi.org/10.2147/ccid.s133672
- Croft, L., Liquori, M., Ladd, J., Day, H., Pineles, L., Lamos, E., … & Morgan, D. (2015). The effect of contact precautions on frequency of hospital adverse events. Infection Control and Hospital Epidemiology, 36(11), 1268-1274. https://doi.org/10.1017/ice.2015.192
- Eriksen, T., Lassen, C., & Gögenur, I. (2014). Treatment with corticosteroids and the risk of anastomotic leakage following lower gastrointestinal surgery: a literature survey. Colorectal Disease, 16(5). https://doi.org/10.1111/codi.12490
- Faith, E., Shah, S., Witman, P., Harfmann, K., Bradley, F., Blei, F., … & Frieden, I. (2021). Clinical features, prognostic factors, and treatment interventions for ulceration in patients with infantile hemangioma. Jama Dermatology, 157(5), 566. https://doi.org/10.1001/jamadermatol.2021.0469
- Hagedorn, J., Pittelkow, T., Hunt, C., D’Souza, R., & Lamer, T. (2020). <p>current perspectives on spinal cord stimulation for the treatment of cancer pain</p>. Journal of Pain Research, Volume 13, 3295-3305. https://doi.org/10.2147/jpr.s263857
- Jain, R., Kim, W., Waldvogel-Thurlow, S., Hwang, P., Cornish, J., & Douglas, R. (2015). The effects of topical agents on paranasal sinus mucosa healing: a rabbit study. International Forum of Allergy & Rhinology, 5(4), 310-317. https://doi.org/10.1002/alr.21470
- Kaufman, K., Mann, F., Kim, D., Lee, S., & Yoon, H. (2014). Evaluation of the effects of topical zinc gluconate in wound healing. Veterinary Surgery, 43(8), 972-982. https://doi.org/10.1111/j.1532-950x.2014.12243.x
- Muñoz, N. and Posthauer, M. (2021). Nutrition strategies for pressure injury management: implementing the 2019 international clinical practice guideline. Nutrition in Clinical Practice, 37(3), 567-582. https://doi.org/10.1002/ncp.10762
- Ojeh, N., Bharatha, A., Gaur, U., & Forde, A. (2020). Keloids: current and emerging therapies. Scars Burns & Healing, 6. https://doi.org/10.1177/2059513120940499
- Politis, C., Schoenaers, J., Jacobs, R., & Agbaje, J. (2016). Wound healing problems in the mouth. Frontiers in Physiology, 7. https://doi.org/10.3389/fphys.2016.00507
- Suter, V., Sjölund, S., & Bornstein, M. (2017). Effect of laser on pain relief and wound healing of recurrent aphthous stomatitis: a systematic review. Lasers in Medical Science, 32(4), 953-963. https://doi.org/10.1007/s10103-017-2184-z
- Wang, J., Ighani, A., Ayala, A., Akita, S., Lara‐Corrales, I., & Alavi, A. (2018). Medical, surgical, and wound care management of ulcerated infantile hemangiomas: a systematic review. Journal of Cutaneous Medicine and Surgery, 22(5), 495-504. https://doi.org/10.1177/1203475418770570
- Wu, Y., Truong, T., Tam, C., Mendoza, M., Zhu, L., Evans, D., … & Fleiszig, S. (2019). Impact of topical corticosteroid pretreatment on susceptibility of the injured murine cornea to pseudomonas aeruginosa colonization and infection. Experimental Eye Research, 179, 1-7. https://doi.org/10.1016/j.exer.2018.10.010
- Zinder, R., Cooley, R., Vlad, L., & Molnár, J. (2019). Vitamin a and wound healing. Nutrition in Clinical Practice, 34(6), 839-849. https://doi.org/10.1002/ncp.10420