Quick Overview
Associated References
Main Article
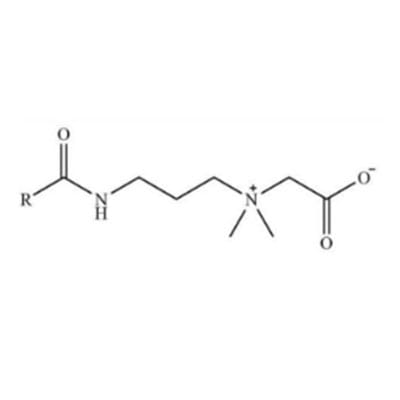
Betaine surfactants, a class of zwitterionic surfactants, have gained significant attention in the field of wound care due to their unique properties and mechanisms that promote healing. Historically, betaine was first identified in sugar beets in the 19th century, but its application in biomedical fields, particularly in wound healing, has only been explored more recently. The increasing prevalence of chronic wounds, such as diabetic ulcers and pressure sores, has necessitated the development of advanced wound care products, including those containing betaine surfactants (Gokarneshan et al., 2015).
The mechanism of action of betaine surfactants in wound healing is multifaceted. These surfactants exhibit excellent hydrophilic properties, which facilitate moisture retention in the wound area, thereby creating a conducive environment for healing (Pereira & Cotas, 2020). The ability of betaine to reduce surface tension enhances the spreadability of topical formulations, allowing for better coverage of the wound bed. This property is particularly beneficial for managing exudative wounds, as it helps to absorb excess fluid while maintaining a moist environment that is crucial for cellular migration and proliferation during the healing process (Violeta et al., 2023).
Betaine surfactants also possess anti-inflammatory properties, which can mitigate the inflammatory response associated with wound healing. By modulating the activity of pro-inflammatory cytokines, betaine can help reduce excessive inflammation that may impede the healing process (Deng et al., 2022). Moreover, studies have indicated that betaine can enhance the proliferation and migration of fibroblasts, which are essential for collagen synthesis and tissue repair (Cherng, 2020). This action is particularly relevant in the context of chronic wounds, where fibroblast activity is often compromised.
In terms of application, betaine surfactants are suitable for various types of wounds, including acute wounds, chronic ulcers, and surgical incisions. Their ability to maintain a moist wound environment makes them particularly effective for managing exuding wounds, such as venous leg ulcers and diabetic foot ulcers (Sahu & Mallick, 2022). Additionally, the incorporation of betaine into wound dressings can enhance the overall performance of these products, providing not only moisture management but also antimicrobial properties that help prevent infection (Vallé et al., 2014).
Recent studies have demonstrated the efficacy of betaine surfactants in promoting wound healing in clinical settings. For instance, a randomized controlled trial found that patients with diabetic foot ulcers treated with betaine-containing dressings exhibited significantly faster healing rates compared to those receiving standard care (Sood et al., 2018). This finding underscores the potential of betaine surfactants as a valuable adjunct in wound management protocols.
Furthermore, the biocompatibility of betaine surfactants makes them an attractive option for wound care applications. Unlike some traditional surfactants that may cause irritation or allergic reactions, betaine is generally well-tolerated by the skin, making it suitable for sensitive wound areas (Paul et al., 2024). This characteristic is particularly important in the context of chronic wounds, where the skin barrier may already be compromised.
In addition to their direct effects on wound healing, betaine surfactants can also enhance the delivery of other therapeutic agents. When incorporated into drug delivery systems, betaine can improve the solubility and stability of active ingredients, thereby enhancing their therapeutic efficacy (Mostolizadeh, 2024). This property opens up new avenues for the development of multifunctional wound dressings that combine the benefits of betaine with other bioactive compounds.
The future of betaine surfactants in wound care looks promising, with ongoing research aimed at optimizing their formulations and exploring new applications. As the understanding of their mechanisms of action continues to evolve, it is likely that betaine surfactants will play an increasingly important role in the management of wounds, particularly in the context of chronic and hard-to-heal ulcers (Kurakula et al., 2020).
In conclusion, betaine surfactants represent a novel and effective approach to wound care, offering a range of benefits that facilitate healing. Their unique properties, including moisture retention, anti-inflammatory effects, and biocompatibility, make them suitable for various wound types. As research progresses, the integration of betaine surfactants into advanced wound care products has the potential to significantly improve patient outcomes and enhance the overall efficacy of wound management strategies.
### The History, Mechanism of Action, and Use of Betaine Surfactant in Wound Care
Betaine surfactants, a class of zwitterionic surfactants, have gained significant attention in the field of wound care due to their unique properties and mechanisms that promote healing. Historically, betaine was first identified in sugar beets in the 19th century, but its application in biomedical fields, particularly in wound healing, has only been explored more recently. The increasing prevalence of chronic wounds, such as diabetic ulcers and pressure sores, has necessitated the development of advanced wound care products, including those containing betaine surfactants (Gokarneshan et al., 2015).
The mechanism of action of betaine surfactants in wound healing is multifaceted. These surfactants exhibit excellent hydrophilic properties, which facilitate moisture retention in the wound area, thereby creating a conducive environment for healing (Pereira & Cotas, 2020). The ability of betaine to reduce surface tension enhances the spreadability of topical formulations, allowing for better coverage of the wound bed. This property is particularly beneficial for managing exudative wounds, as it helps to absorb excess fluid while maintaining a moist environment that is crucial for cellular migration and proliferation during the healing process (Violeta et al., 2023).
Betaine surfactants also possess anti-inflammatory properties, which can mitigate the inflammatory response associated with wound healing. By modulating the activity of pro-inflammatory cytokines, betaine can help reduce excessive inflammation that may impede the healing process (Deng et al., 2022). Moreover, studies have indicated that betaine can enhance the proliferation and migration of fibroblasts, which are essential for collagen synthesis and tissue repair (Cherng, 2020). This action is particularly relevant in the context of chronic wounds, where fibroblast activity is often compromised.
In terms of application, betaine surfactants are suitable for various types of wounds, including acute wounds, chronic ulcers, and surgical incisions. Their ability to maintain a moist wound environment makes them particularly effective for managing exuding wounds, such as venous leg ulcers and diabetic foot ulcers (Sahu & Mallick, 2022). Additionally, the incorporation of betaine into wound dressings can enhance the overall performance of these products, providing not only moisture management but also antimicrobial properties that help prevent infection (Vallé et al., 2014).
Recent studies have demonstrated the efficacy of betaine surfactants in promoting wound healing in clinical settings. For instance, a randomized controlled trial found that patients with diabetic foot ulcers treated with betaine-containing dressings exhibited significantly faster healing rates compared to those receiving standard care (Sood et al., 2018). This finding underscores the potential of betaine surfactants as a valuable adjunct in wound management protocols.
Furthermore, the biocompatibility of betaine surfactants makes them an attractive option for wound care applications. Unlike some traditional surfactants that may cause irritation or allergic reactions, betaine is generally well-tolerated by the skin, making it suitable for sensitive wound areas (Paul et al., 2024). This characteristic is particularly important in the context of chronic wounds, where the skin barrier may already be compromised.
In addition to their direct effects on wound healing, betaine surfactants can also enhance the delivery of other therapeutic agents. When incorporated into drug delivery systems, betaine can improve the solubility and stability of active ingredients, thereby enhancing their therapeutic efficacy (Mostolizadeh, 2024). This property opens up new avenues for the development of multifunctional wound dressings that combine the benefits of betaine with other bioactive compounds.
The future of betaine surfactants in wound care looks promising, with ongoing research aimed at optimizing their formulations and exploring new applications. As the understanding of their mechanisms of action continues to evolve, it is likely that betaine surfactants will play an increasingly important role in the management of wounds, particularly in the context of chronic and hard-to-heal ulcers (Kurakula et al., 2020).
In conclusion, betaine surfactants represent a novel and effective approach to wound care, offering a range of benefits that facilitate healing. Their unique properties, including moisture retention, anti-inflammatory effects, and biocompatibility, make them suitable for various wound types. As research progresses, the integration of betaine surfactants into advanced wound care products has the potential to significantly improve patient outcomes and enhance the overall efficacy of wound management strategies.
References
- Mcqueen, R., et al. (2018). Parameter Search to Find Ranges of Activation and Inhibition of Wound Healing Rate in a Mathematical Model with Introduced Photobiomodulation. *Springer*. Available at: https://doi.org/10.1007/978-981-10-9035-6_151, Accessed 28 December 2024
- Ovington, L. (2023). Surgical Wound Closure and Healing. *IntechOpen*. Available at: https://doi.org/10.5772/intechopen.105978 , Accessed 28 December 2024
- Musa, A. and Min, T. (2022). Haruan Extract (Channa striatus) as an Effective Mediator in Promoting Wound Healing. *IntechOpen*. Available at: https://doi.org/10.5772/intechopen.99207 , Accessed 28 December 2024
- Ručigaj, T. (2021). Skin Wound Healing. *Springer*. Available at: https://doi.org/10.1007/978-3-319-53811-2_8 , Accessed 28 December 2024
- Dwivedi, C. and Lepková, K. (2017). SAXS and SANS Techniques for Surfactant Characterization: Application in Corrosion Science. *IntechOpen*. Available at: https://doi.org/10.5772/intechopen.69290 , Accessed 28 December 2024
- Bruwer, A. (2024). Amniotic Membrane in the Treatment of Hard-to-Heal Wounds. *IntechOpen*. Available at: https://doi.org/10.5772/intechopen.1004843 , Accessed 28 December 2024
- Brand, H., et al. (2014). Saliva and Wound Healing. *Karger Publishers*. Available at: https://doi.org/10.1159/000358784 , Accessed 28 December 2024
- Gould, L., et al. (2020). Evidence Supporting Wound Care End Points Relevant to Clinical Practice and Patients’ Lives. Part 3: The Patient Survey. *Wound Repair and Regeneration*, 28(4), pp. 451-459. Available at: https://doi.org/10.1111/wrr.12872, Accessed 28 December 2024
- Mikolka, P., et al. (2016). Antiinflammatory Effect of N-Acetylcysteine Combined with Exogenous Surfactant in Meconium-Induced Lung Injury. *Springer*. Available at: https://doi.org/10.1007/5584_2016_15 , Accessed 28 December 2024
- Flores-Escobar, J. (2024). Low-Frequency Contact Ultrasonic Debridement in Diabetic Foot Ulcer. *IntechOpen*. Available at: https://doi.org/10.5772/intechopen.1004066 , Accessed 28 December 2024
- Soni, A., et al. (2023). Nanotechnological Interventions and Mechanistic Insights into Wound-Healing Events. *IntechOpen*. Available at: https://doi.org/10.5772/intechopen.106481 , Accessed 28 December 2024